Low vitamin D status: who is at risk?
Neil R. Brett, PhD
PhD, Postdoctoral Fellow School of Nutrition, Ryerson University, Toronto, Canada
Recommendations for Vitamin D
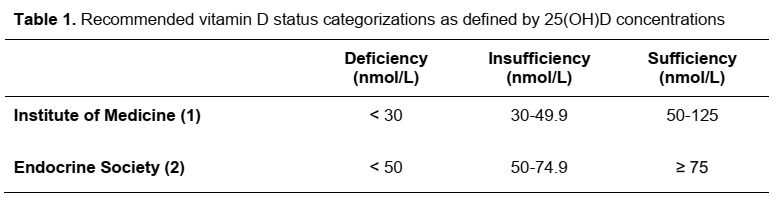
Vitamin D is well accepted for its function in bone health, as well as having roles in muscle function and general health. Vitamin D cannot be endogenously synthesized year round in regions above 40ο N latitude and thus, vitamin D is considered an essential nutrient [1]. Institute of Medicine (IOM) and the Endocrine Society vitamin D status recommendations were set for bone health outcomes (Table 1). They differ due to differences in studies included in the review processes, outcomes of interest and interpretation of data. When looking at other outcomes than bone health, vitamin D status > 75 nmol/L is commonly used to define sufficiency. However, more work is needed to set specific recommendations for vitamin D-related outcomes including immune health and muscle health.
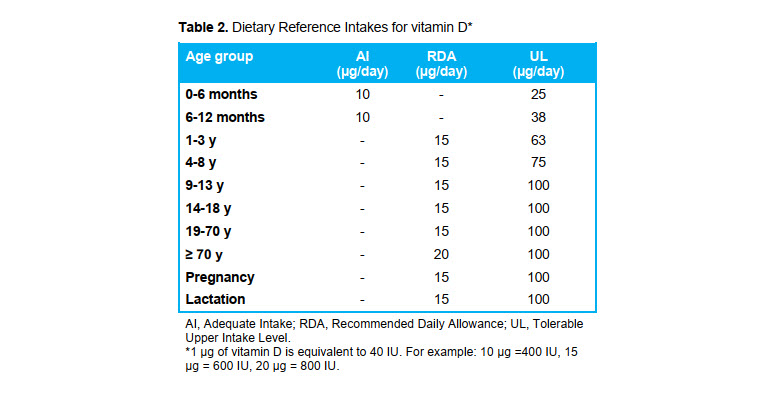
The IOM guidelines for vitamin D status (Table 1) were set to align with North American vitamin D intake recommendations (Table 2), where consuming the Recommended Dietary Allowance (RDA) for vitamin D is designed to align with a sufficient vitamin D status. However, vitamin D intakes and statuses of Americans and Canadians don’t seem to be well aligned as < 20% meet the RDA whilst roughly 2/3 have sufficient vitamin D status. Few foods contain vitamin D and there are many factors affecting vitamin D status. Thus, this article will discuss the factors affecting vitamin D status to help clarify how much vitamin D people should consume and who is at a higher risk for vitamin D deficiency.
Factors affecting endogenous vitamin D production from UV-B radiation
Though midday sun exposure for 10–30 minutes twice per week may be adequate for production of vitamin D [3], recommendations are to limit UV exposure, especially for children. This is because UV radiation has been linked to premature aging, skin cancer, eye problems, sun burns and weakening of the immune system [4]. Because of this and because of the multiple factors, listed below, contributing to inconsistent or minimal UV-B exposure, vitamin D intake guidelines were set to be sufficient in the absence UV-B exposure.
-
Latitude: Living further from the equator means that there are fewer months of the year that sunlight contains sufficient quantities of UV-B rays to support vitamin D synthesis in the skin. In Canada, there is minimal vitamin D synthesis between October-March.
-
Time of day: During the months that vitamin D can be synthesized, roughly 10 am to 4 pm are the hours when vitamin D can be synthesized. Thus, working an indoor 9 am to 5 pm job means that you will not be able to get much vitamin D synthesis on workdays.
-
Elevation: Higher altitude increases the amount of UV-B radiation that individuals are exposed to because of lower atmospheric density. A recent review paper stated that for every increase of 300 meters of altitude, UV-B radiation exposure increases by around 4% [3].
-
Skin colour: As skin pigment (melanin) acts to limit the amount of UV-B radiation that can be used to produce vitamin D, darker skin colour (more melanin) results in less endogenous vitamin D production form UV-B.
-
Age: As people get older, the efficiency of vitamin D synthesis decreases. For example, vitamin D synthesis is only possible when exposed to sunlight between 10 am and 3 pm [5]. For example, people over the age of 70 years have been shown to synthesize 25% less vitamin D from exposure to sunlight when compared to 20 year olds [5], whilst 8 year old children were shown to synthesize 20% more vitamin D compared to 18 year olds [6].
-
Sunscreen use and clothing worn: Proper sunscreen use or clothing covering most skin can both minimize UV-B exposure and vitamin D synthesis. For example, multiple sunny global regions, where it is typical for individuals to be fully covered in clothing, have average vitamin D status below 50 nmol/L [7].
-
Pollution: Areas with higher levels of air pollution have been shown to decrease the ability of UV rays to reach the skin to produce vitamin D [3], resulting in lower average vitamin D status of the population.
Other factors affecting vitamin D status
-
Food versus supplements: Based on a recent review paper focused on pediatric populations, it is possible that vitamin D from food sources, compared to supplements, has a greater ability to increase vitamin D status [8]. For food sources of vitamin D, this review paper only included fortified foods, but it is likely that foods naturally containing vitamin D would have a similar affect.
-
Daily versus bolus: It is likely that consuming vitamin D regularly (i.e. 400-600 IU daily or 1000 IU multiple times per week) is more efficacious than taking sporadic large doses of vitamin D [8].
-
Vitamin D2 versus D3: Vitamin D3 is the common form of the vitamin found in supplements and is the form in animal products likely fatty fish. Vitamin D2 is found in irradiated mushrooms and possibly from other fungi or yeast. Vitamin D3 is likely more effective than D2 for raising vitamin D status [9].
-
Weight status: Individuals who are overweight or obese are at a higher risk of vitamin D deficiency [10]. This is likely because adipose tissue is the principal storage site of vitamin D [11], meaning that greater adiposity causes more vitamin D to be taken out of circulation and stored. Further, individuals with a large amount of muscle mass may also need a greater vitamin D intake as it has been estimated, in adults, that ~ 20% of 25(OH)D is in muscle tissue [11].
-
Genetic factors: A number of genetic variants affect enzymes and processes involved in vitamin D synthesis and metabolism [12, 13]. These factors are not routinely measured but are an important reason why some people need a higher vitamin D intake to maintain a sufficient vitamin D status.
Summary and take-away points
Limiting UV exposure is recommended, however, UV-B exposure still contributes to total vitamin D intake for many individuals. Inconsistent or limited exposure means that vitamin D should be consumed from the diet. Though foods like fatty fish and fortified dairy or cereals contain vitamin D, people do not routinely consume enough to meet the recommended intakes.
-
For healthy individuals, meeting the RDA (Table 2) should be adequate to maintain a sufficient vitamin D status. To meet the RDA, supplements may be needed, however, this should be assessed on an individual basis.
-
For populations at higher risk of vitamin D deficiency (i.e. individuals with obesity), vitamin D intakes may need to be double the RDA to maintain a sufficient vitamin D status [2]. Having vitamin D status measured in these populations may be useful, but the need for measurement should be considered on an individual basis with an understanding of individual risk factors for vitamin D deficiency.
Show your client the sources of vitamin D in their diet with Keenoa.