Calcium supplements: friend or foe?
Angel Ong, RD, MSc
Registered dietitian, MSc, PhD candidate McGill University
Calcium and bone integrity
Calcium is an abundant mineral in the body that plays a pivotal role in bone mineralization. Approximately 99% of the body’s calcium is stored in the bones and teeth. The remaining calcium is found in the circulatory system, extracellular fluid, muscle, and other tissues where it is critical for extra-skeletal functions. The skeleton therefore acts as a reservoir of calcium for metabolic function needs such as contraction, vasodilation, muscle function, nerve transmission, intracellular signaling, and hormonal secretion.
The bone is a dynamic organ and undergoes constant remodeling to remove old bone (resorption) and to replace it with new ones (formation). When bone resorption exceeds bone formation, then bone loss occurs, predisposing the individual to osteoporosis. This phenomenon can be observed in older adults as a result of age-related bone loss.
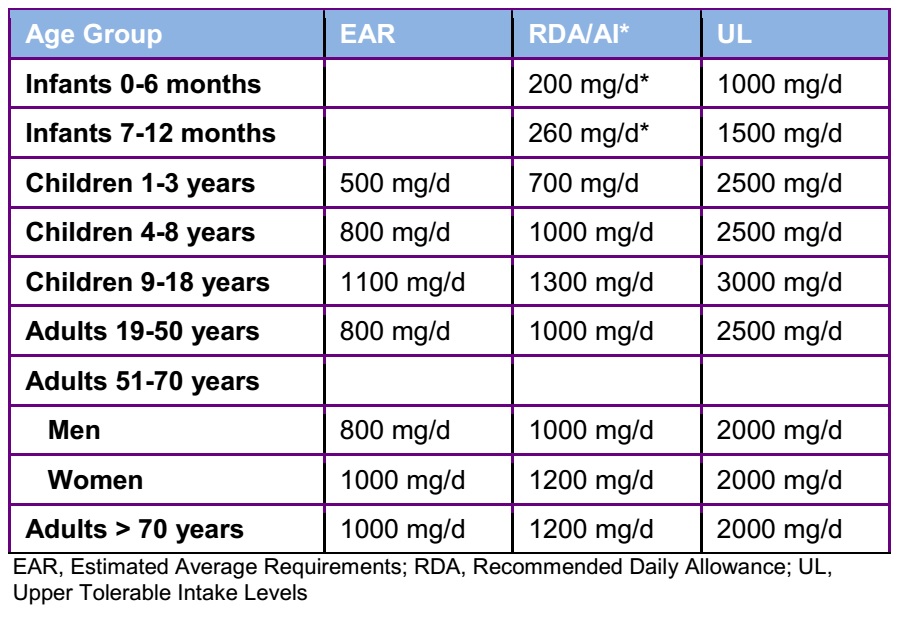
The current Dietary Reference Intakes for calcium are higher for women over the age 50 and men over 70, as compared to adults of the same sex in the lower age bracket, to reflect the accelerated bone loss in older adults (Table 1) [1].
Table 1: Dietary Reference Intakes for Calcium
Major sources of dietary calcium in the North American diet consist of milk and milk products as well as some non-dairy foods. However, the recommended intakes of calcium can be difficult to achieve through dietary sources alone especially in older adults. Reports of national surveys revealed that less than 10 % of Americans and Canadians over 50 years of age had an intake above 1000 mg/day [2, 3]. To minimize age-related bone loss, dietary supplements of calcium can be helpful for older adults to achieve an adequate intake of calcium. A daily vitamin D intake of 800 IU is also recommended for bone health for adults older than 50 years of age. Individuals with osteoporosis, history of fragility fractures, or conditions affecting vitamin D absorption could require up to 2000 IU of vitamin D per day.
Calcium supplements are generally well tolerated, but can be associated with mild gastrointestinal symptoms and, rarely, with renal lithiasis [4]. However, recommendation of calcium supplements for the prevention and management of osteoporosis has become a controversial topic in clinical practice.
Conflicting evidence
The discussion regarding the safety of calcium supplement use began in 2010, following the publication of a meta-analysis that was published in the British Medical Journal. The authors pooled 15 placebo-controlled trials of calcium, without co-administration of vitamin D, and found a 31% increased risk of myocardial infarction with calcium supplement use [5]. The same authors published another meta-analysis the following year to include trials of calcium with vitamin D co-administration to address the important limitations in the methodology of their previous report [6]. The increased risk for myocardial infarction associated with calcium supplement use remained (relative risk of 1.24, 95% confidence interval 1.07 to 1.45), but there were other concerns related to the methodology of their report. Subsequent meta-analyses that were undertaken by other research groups addressing important considerations found no association between calcium supplementation and cardiovascular risk [7, 8].
Furthermore, none of the studies included in the previous reports had cardiovascular events as their primary endpoint. Despite the lack of clinical trials investigating the effect of calcium supplement on cardiovascular disease outcomes as primary endpoints, it would be unethical for such a study design to be conducted.
Still, it remains important to understand the underlying mechanism of the potential effect of calcium supplements on cardiovascular health. A randomized controlled trial is being undertaken at the Research Institute of McGill University to investigate whether calcium supplements have a different effect on surrogate markers of vascular health in healthy postmenopausal women compared to dietary sources of calcium (ClinicalTrials.gov ID: NCT01731340). Participants are randomized to one of three groups for 1-year trial:
- Group 1 (Calcium Supplement): 750 mg calcium supplement with 450 mg calcium from food sources and a vitamin D supplement (800 IU/d)
- Group 2 (Dietary Calcium): 1200 mg calcium from food sources with a vitamin D supplement (400 IU/d)
- Group 3 (Usual Diet): Continue their usual diet with a vitamin D supplement (400 IU/d).
Innovative and non-invasive technology is used to measure the arterial stiffness and carotid intima-media thickness to capture vascular change caused by calcium at an early stage before the development of cardiovascular events. Results from this clinical trial will provide insights into the mechanisms that may be responsible for the changes observed and will add to the current body of knowledge.
The bottom line: is it safe or not?
In light of the evidence available to date, the National Osteoporosis Foundation and the American Society for Preventive Cardiology recently adopted a joint position that there is moderate-quality evidence that total calcium intake, from supplements and dietary sources, with or without vitamin D, that does not exceed the Upper Tolerable Intake Levels should be considered safe from a cardiovascular standpoint [9].
Patients should be encouraged to obtain most of their calcium from food sources to also obtain other nutrients for bone health as compared to only getting calcium from supplements.
Take home message
- Adequate calcium and vitamin D intake throughout adulthood are important modifiable factors in ensuring bone health to prevent osteoporosis.
- Most adults, especially the elderly, fail to meet the current recommendations for calcium through food sources only.
- Calcium supplements can help close the gap from dietary intakes. There is moderate-quality evidence suggesting that calcium intake from calcium supplements and dietary calcium below the Upper Tolerable Intake Levels is considered safe for cardiovascular health.
- Prior to recommending a calcium supplement, it is important to first evaluate the individual’s usual dietary calcium intake over several days.
Is your client meeting the calcium recommendations through their diet? Learn how Keenoa can help.